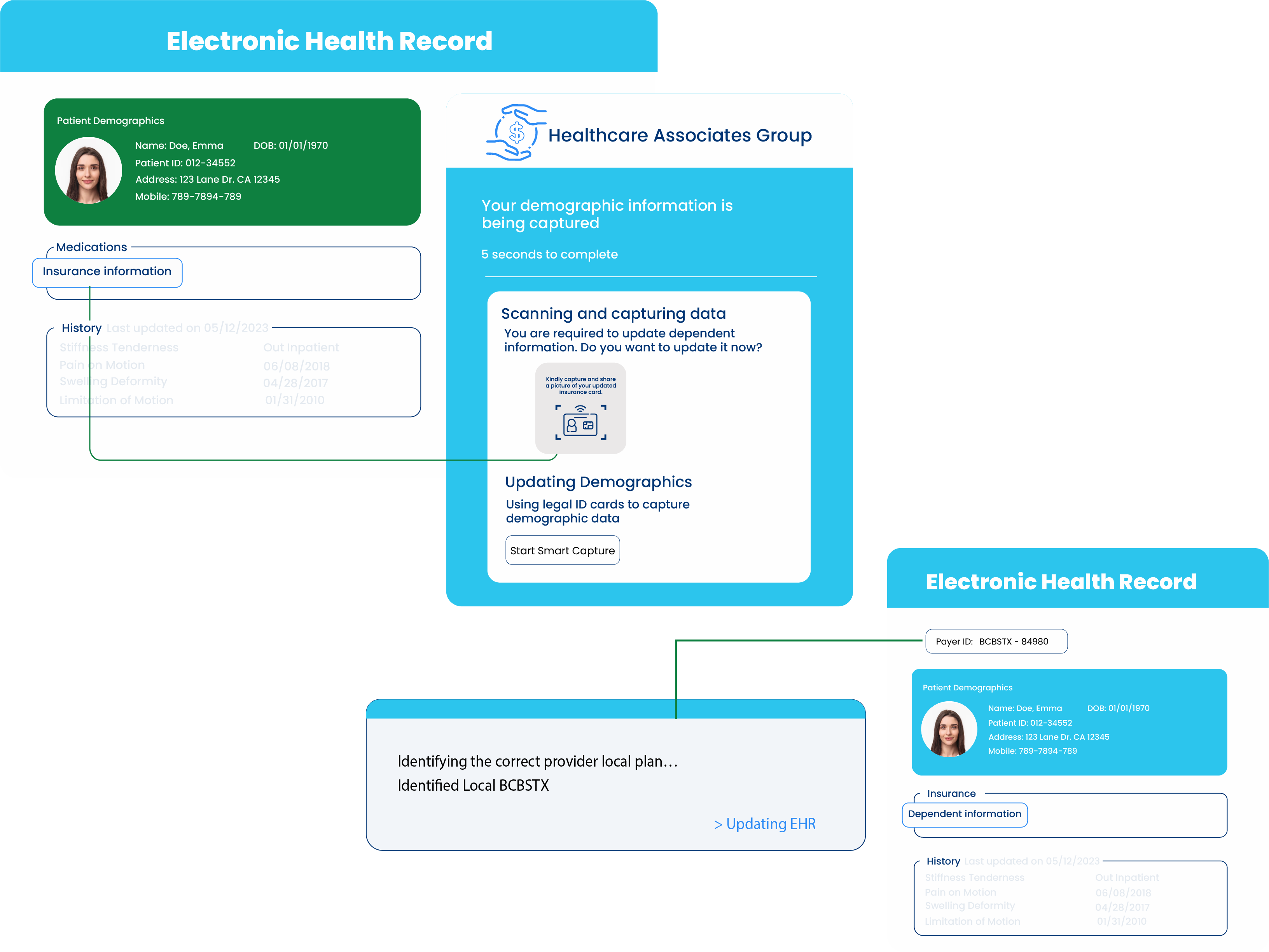
Eliminate Data Capture Mistakes
27% of all denied claims stem from inaccurate patient demographics, avoidable with our AI insurance card reader.
HIPAA Compliant
Every piece of data processed by the AI is secured using PHI protection algorithms that comply with HIPAA standards, ensuring a 0% risk of data breaches.
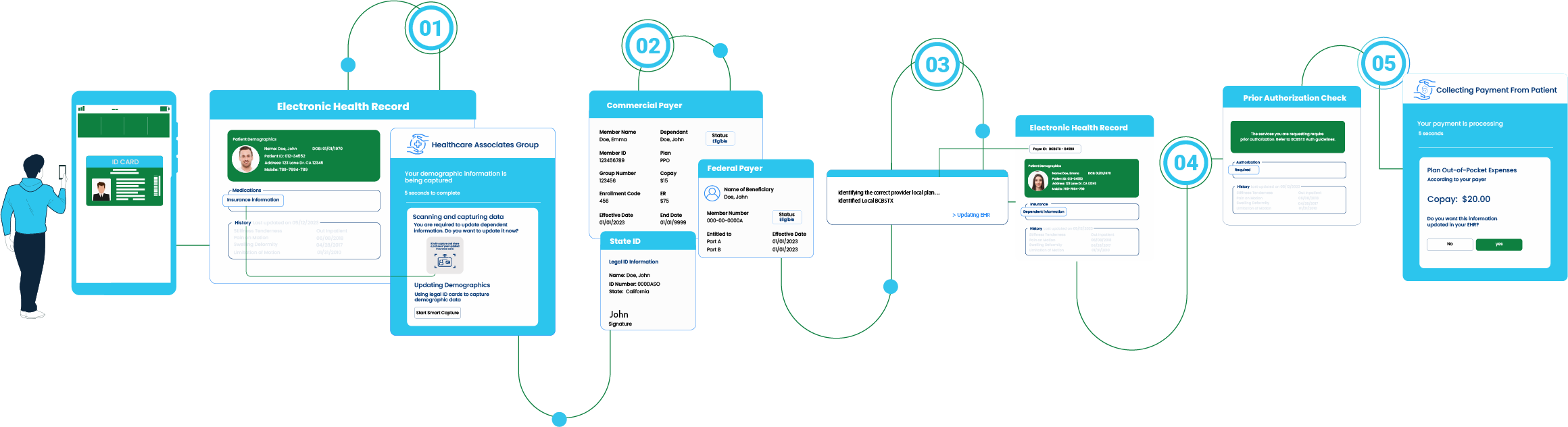
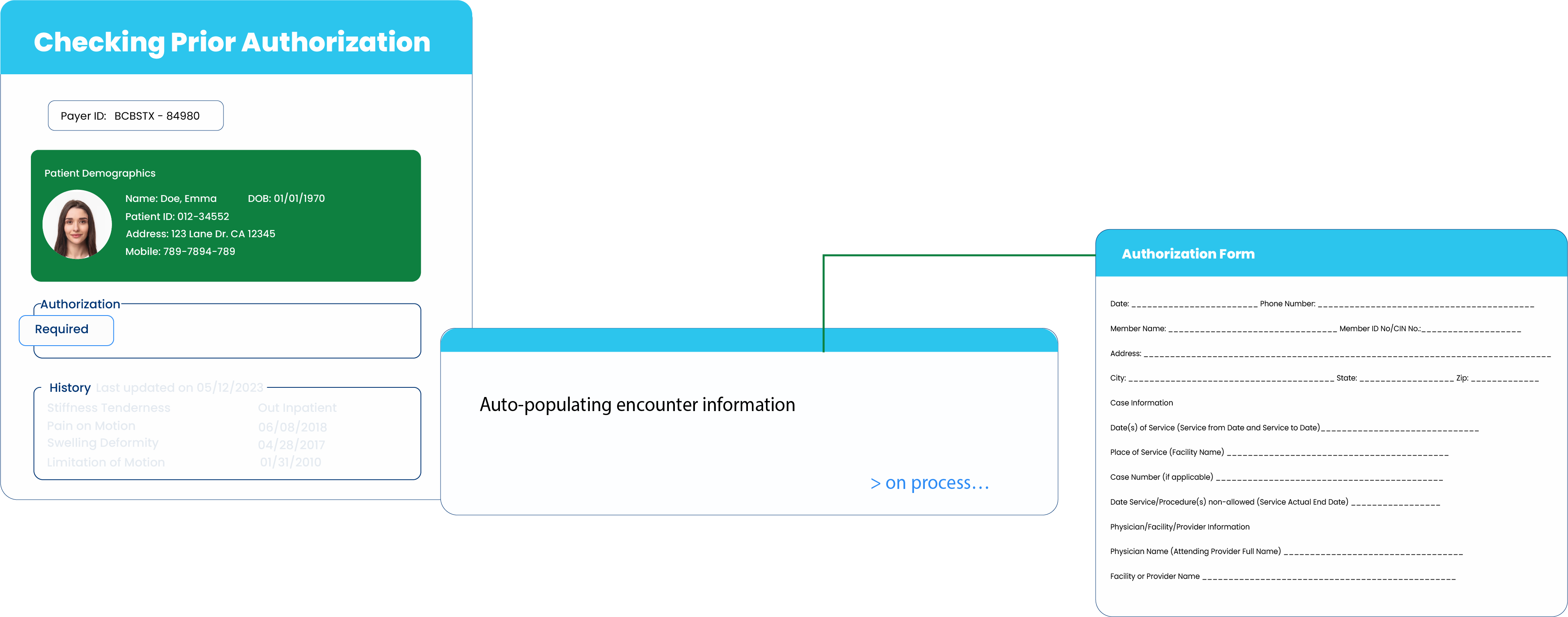
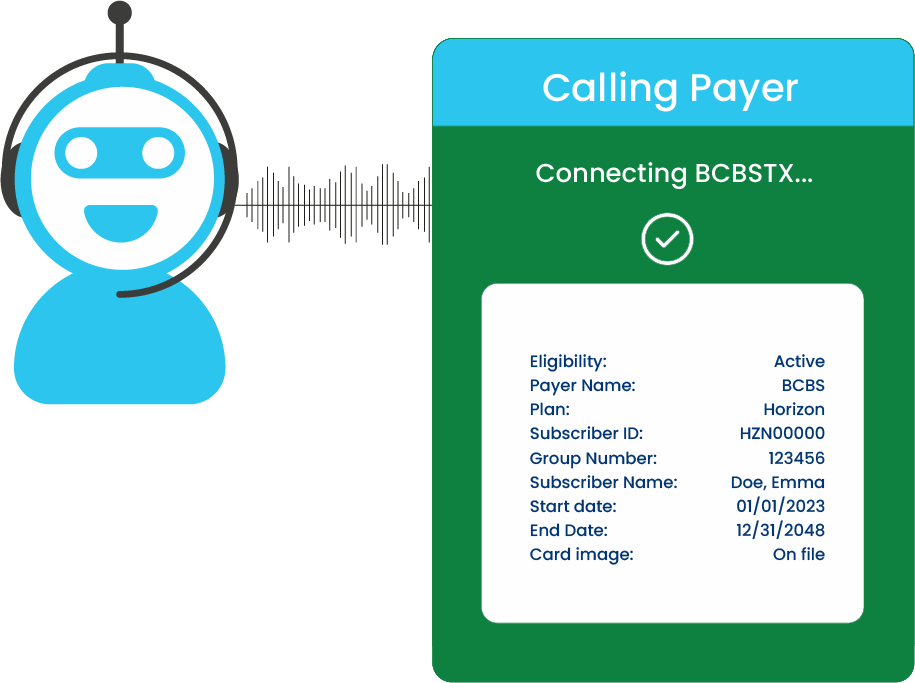
Increase Productivity
With our AI bots handling the heavy lifting, your front office staff can offer essential support for your patients, enhancing the care experience.
AI-Powered Rest API/SDK
Two secure capture methods through RestAPI/SDK, featuring Azure CDN for client-side optimization and AI-enhanced server-side accuracy.