Prior Authorization
Determines if prior authorization is required
Our authorization determination engine automatically determines if a prior authorization is required or not with accuracy by referring to the payer guidelines and CPT code of the service.
Authorization Inquiry / Status
Automated repeated follow-up with payers and real-time status updates are provided by our APIs, EDI, and RPA bots. Real-time status updates help your staff keep patients informed and procedures get scheduled on time.
Create Case / Requests / Submission
Create new cases, and sort through the cases intuitively with the help of several filters, search and sort options.
Organizations We Serve
General Provider
Ambulatory Surgery
EMR/PMS
Oncology
Radiology
Labs
Pain Management
Gastroenterology
Payer Connections
EMR/PMS Connections
Plan Members
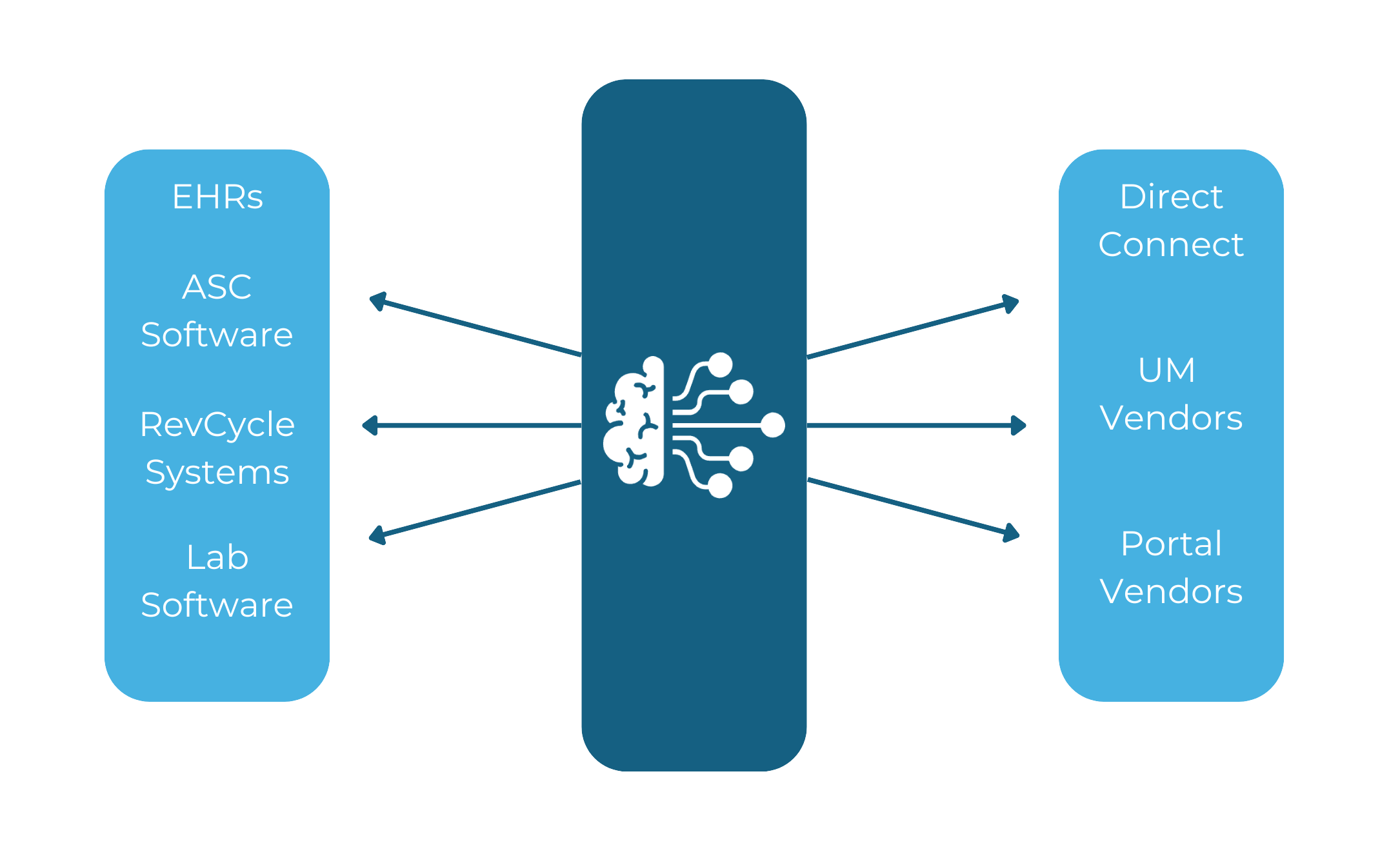
Autonomous Integrations and Workflow
ORBIT Connectivity Suite
HL7 V2 to FHIR
HL7 V2 ADT data flow begins from any provider site
HL7 V2 (or JSON-wrapped ADT) into a FHIR R4 Patient Resource JSON object and delivers the JSON payload to the API endpoint

FHIR to FHIR
Requests made over secure connection for data via FHIR R4 resource
FHIR R4 messages relayed into central FHIR R4 repository

Database to HL7
Requests made over secure connection for data via SQL query messages
SQL messages transformed into HL7 V2 messages
Custom API to FHIR or HL7
API input messages retrieved and transformed into FHIR R4
Messages relayed into central FHIR R4 repository or HL7 V2 feed