Lessons Learned from the Change Healthcare Outage
Lessons Learned from the Change Healthcare Clearinghouse Outage. Why Payer Gateway Connection Redundancy is More Important Than Ever
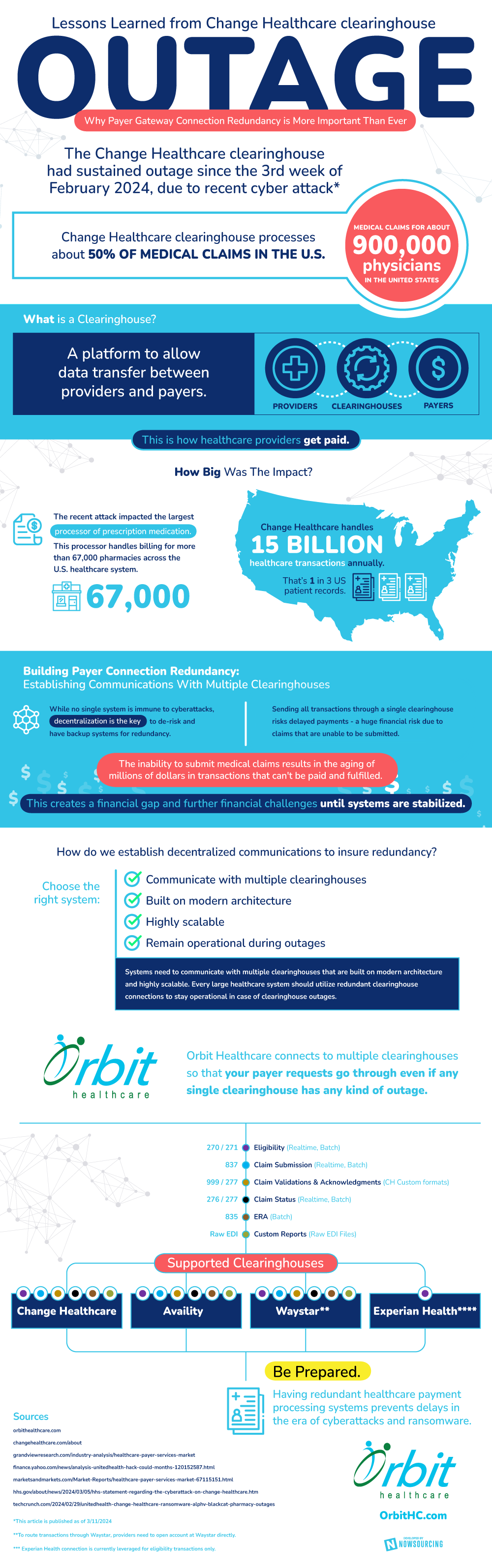
The Change Healthcare clearinghouse had sustained outage since the 3rd week of February 2024, due to recent cyber attack*
Change Healthcare clearinghouse processes about 50% of medical claims in the U.S. (Medical claims for about 900,000 physicians in the United States
What is a Clearinghouse?
A platform to allow data transfer between providers and payers. This is how healthcare providers get paid.
How Big Was The Impact?
The recent attack impacted the largest processor of prescription medication. This processor handles billing for more than 67,000 pharmacies across the U.S. healthcare system. Change Healthcare handles 15 billion healthcare transactions annually – That’s 1 in 3 US patient records.
Building Payer Connection Redundancy:
Establishing Communications With Multiple Clearinghouses
While no single system is immune to cyberattacks, decentralization is the key to de-risk and have backup systems for redundancy.
Sending all transactions through a single clearinghouse risks delayed payments – a huge financial risk due to claims that are unable to be submitted.
The inability to submit medical claims results in the aging of millions of dollars in transactions that can’t be paid and fulfilled. This creates a financial gap and further financial challenges until systems are stabilized.
How do we establish decentralized communications to insure redundancy?
Choose the right system:
- Communicate with multiple clearinghouses
- Built on modern architecture
- Highly scalable
- Remain operational during outages
Systems need to communicate with multiple clearinghouses that are built on modern architecture and highly scalable. Every large healthcare system should utilize redundant clearinghouse connections to stay operational in case of clearinghouse outages.
Orbit Healthcare connects to multiple clearinghouses so that your payer requests go through even if any single clearinghouse has any kind of outage.
270 / 271 – Eligibility (Realtime, Batch)
837 – Claim Submission (Realtime, Batch)
999 / 277 – Claim Validations & Acknowledgments (CH Custom formats)
276 / 277 – Claim Status (Realtime, Batch)
835 – ERA (Batch)
Custom Reports (Raw EDI Files)
Supported Clearinghouses:
- Change Healthcare
- Availity
- Waystar**
- Experian Health****
Be Prepared. Having redundant healthcare payment processing systems prevents delays in the era of cyberattacks and ransomware.
Sources
grandviewresearch.com/industry-analysis/healthcare-payer-services-market
finance.yahoo.com/news/analysis-unitedhealth-hack-could-months-120152587.html
marketsandmarkets.com/Market-Reports/healthcare-payer-services-market-67115151.html
hhs.gov/about/news/2024/03/05/hhs-statement-regarding-the-cyberattack-on-change-healthcare.htm
techcrunch.com/2024/02/29/unitedhealth-change-healthcare-ransomware-alphv-blackcat-pharmacy-outages
*This article is published as of 3/11/2024
**To route transactions through Waystar, Providers need to open account at Waystar directly.
*** Experian Health connection is currently leveraged for eligibility transactions only.
